Britain has abandoned a £75m plan to make vital items of reusable protective clothing to guard against a second wave of Covid-19, denting hopes of concerted government action to promote sustainable manufacturing, and triggering dismay among industry observers.
Above: Protective gowns are mostly discarded after one use, adding to the UK’s waste mountain
The millions of protective gowns for health workers would have come from UK factories and could have been reused up 100 times each.
Most protective garments are imported from low-cost nations and discarded after one wearing, conflicting with environmental goals.
But three months of talks between industry representatives and the Cabinet Office – responsible for key government policies – have ground to a halt after officials failed to agree the details of the scheme.
Adam Mansell, chief executive of the UK Fashion & Textile Association, representing manufacturers, designers and suppliers, said: “There had been a fantastic opportunity for the government to tap into Britain's technical expertise on textiles to set up a sustainable supply of reusable gowns made in the UK. The way the government has handled this project has been poor and says little for its commitment to help UK manufacturing."
Yvette Ashby, chief executive of the Professional Clothing Industry Association Worldwide, a London-based trade body, said: “The people working on this [in the Cabinet Office] appear to have little understanding of how the textile industry works. Their approach has sometimes appeared chaotic. A lot of people from industry are pretty frustrated with the lack of response.”
Since the scheme would have safeguarded jobs in UK textiles businesses, many of which are in economically depressed regions, it would have supported Boris Johnson’s “levelling up” theme. In this the prime minister has talked about helping poorer regions catch up with the rest of the UK during an anticipated economic rebound.
The discussions ended after officials realised that, following protracted delays in agreeing the scheme, many individual health trusts had placed their own local orders for gowns, reducing the need for a centralised project.
Many of the gowns topping up local supplies are imported and disposable. Local efforts fail to capture the economies of scale and adherence to rigid quality standards that a centralised programme would have entailed.
The UK has more than 200 health trusts organising regional services in conjunction with centralised parts of the National Health Service and the Department of Health and Social Care.
The failure of the talks has sparked disquiet at two big companies that were to have played a big part in the scheme - online retailer Asos and the UK arm of Japanese textiles producer Toray. Asos would have acted as project manager, organising production of up to 5m gowns over a year from a network of UK plants, while Toray would have supplied most of the specialised fabric needed for the gowns from a plant near Nottingham.
 Toray’s factory in Mansfield would have played a key part in the project
Toray’s factory in Mansfield would have played a key part in the project
At the peak of the pandemic protective gowns were required in enormous numbers in hospitals yet were in short supply. Deficiencies across all types of personal protective equipment are regarded as one reason for Britain’s high death rate.
The ending of the talks – in which the Deloitte consultancy supported the Cabinet Office – has not been announced by the government.
After being criticised early in the pandemic for slow progress in addressing PPE shortages, ministers and officials have been keen to demonstrate its efforts are gaining traction.
On June 25, the DHSC said it had ordered from UK and overseas suppliers some 28bn PPE items to tackle coronavirus, as “part of herculean cross-government effort to future-proof supply chains”. About 2bn of the items would be made in the UK, according to a previous announcement in May. By the end of 2020, “around 20 per cent” of all PPE used in Britain would be manufactured domestically, the DHSC has said.
However, the department has not broken out which items of PPE feature in these figures, nor given details of more than a handful of contracts. The government counts as PPE items as diverse as body bags, paper towels and cleaning equipment. The Treasury has set aside £15bn to pay for PPE, roughly a fifth of the NHS’s total procurement bill in England in 2018/19.
The DHSC said: “We are working with Public Health England, NHS England and Improvement, and the Health and Safety Executive to look at strategies for optimising the supply of PPE. All PPE must meet our rigorous standards to ensure staff and patient safety.” The DHSC, Cabinet Office, Asos and Deloitte declined to comment on the discussions over reusable gowns.
How a green manufacturing model fell apart
The government’s discussions over reusable protective gowns started out as an impressive attempt to combine two ideas – shifting the emphasis in a key area of personal protective equipment from disposable to renewable and boosting domestic manufacturing at a time of economic stress.
In the end neither goal was met, leaving industry figures who took part in the discussions disappointed.
David Stevens, chief executive of the Textiles Services Association, representing laundries that would have played a big part in recycling the gowns by washing each one 40-100 times, said the centralised plan would have made “a lot of sense from both an environmental and economic perspective”. It was “disappointing and frustrating” that so little progress had been made.
According to people involved with the talks, the cost of the project would have been about £75m. Online retailer Asos – best known for its fashion clothing and with no plants of its own but a good reputation for manufacturing knowhow – would have acted as project manager.
The conversations between the Cabinet Office and industry representatives followed criticism in March and April that the government had failed to build up stocks of PPE.
Shortages of gowns and related items in hospitals and care homes have been widely blamed for the rapid early spread of the virus, leading to a high official death rate of more than 41,000. This makes the UK the fifth-worst on this measure in the world, behind the US, Brazil, Mexico and India.
The effort to set up a UK-wide scheme for reusable gowns was handed to Lord Paul Deighton, a former Goldman Sachs banker and head of the organising committee for the 2012 London Olympics. Deighton was appointed in April to take charge of PPE purchasing, operating from the Cabinet Office – the government’s central policy body.
Deighton and Moira Ford, a procurement specialist who was part of his team, modelled the reusables project on a related government scheme on protective gowns organised in March, prior to his appointment.
Under this scheme roughly 6m single-use gowns are being made by five UK textiles makers using material supplied by a plant in Forfar, Scotland, run by Don & Low, a Greek-owned textiles firm. The cost of this programme is put at about £50m.
The individual manufacturers involved with the Don & Low project include Preston-based BB Workwear; Keela, based in Glenrothes, Scotland; Private White VC, a known mainly for its fashion clothing with a factory in Manchester; Survitec, in Birkenhead; and Redwood TTM which has several plants in Lancashire.
 The Keela clothes maker is among several UK plants involved in an earlier UK scheme to make disposable gowns
The Keela clothes maker is among several UK plants involved in an earlier UK scheme to make disposable gowns
While BB Workwear plans to make 2.5m gowns during 2020, many which are part of the Don & Low project, Redwood TTM is making 850,000. Mike Stoll of Private White VC – which is making 1.1m gowns under the Don & Low scheme, said: “The government should be backing the idea of making more textiles products in the UK. It provides employment and gives the country a payback through taxation. It makes sense in the longer term.”
Samantha Fernando, sales director at Keela, which is making more than 500,000 gowns under the Don & Low scheme, said it was “fantastic” that officials had organised this “to support British manufacturing”.
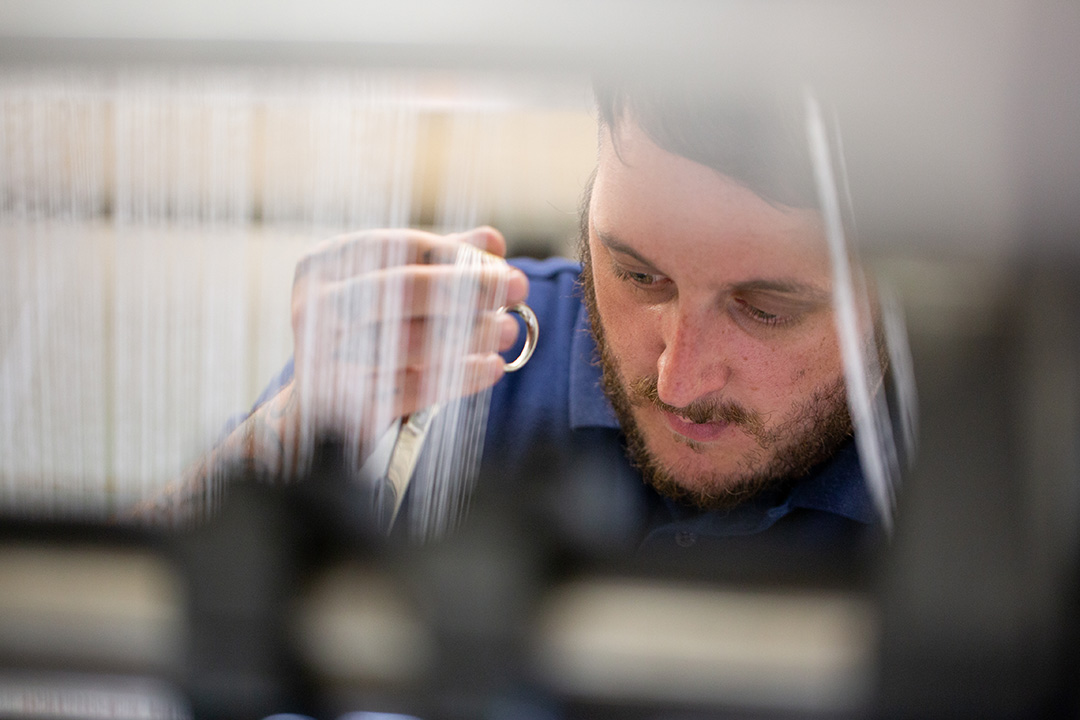
 One of Keela’s 100 employees in its Glenrothes plant - whose main product is specialised outdoor clothing
One of Keela’s 100 employees in its Glenrothes plant - whose main product is specialised outdoor clothing
Also participating in the cabinet office talks on the reusables programme were officials from the public purchasing agency Crown Commercial Service, the Department of Health and Social Care, the Department of Business, Energy and Industrial Strategy and NHS Improvement (responsible for mapping long-term health policy).
A vital part of the new project involved laundry companies, which would be required to stick to rigorous standards when cleaning the gowns between uses. Large laundries including those run by two big companies, Elis and Synergy, would have played a central role.
Unlike in the Don & Low project, where the DHSC and the Scottish government between them organised the production of gowns by individual businesses, for the new scheme Deighton and Ford wanted to find one big company to which they could entrust the project management.
In the absence of any large suitable UK manufacturer they identified Asos. The clothing retailer relies on a global network of contractors to make its garments. It is well regarded for its record on sustainability and ensuring suppliers treat workers fairly. Out of its 173 suppliers in 24 countries, 24 are in the UK.
Working with the cabinet office, Simon Platts, Asos’s sourcing director, organised a group of its UK suppliers that could make the gowns. Mick Cheema, general manager of Basic Premier, an Asos supplier based in Leicester which worked on the scheme, said he had high hopes for the programme as creating a “new focus for UK manufacturing” in health-related procurement.
But efforts to finalise the scheme petered out after the cabinet office baulked at the likely costs of the project. Asos would have received about £15 a gown. This is considerably more (ignoring any benefits related to sustainability) than the unit costs of comparable disposable items bought from overseas. Asos would have made little profit on its involvement, say people involved.
It appears officials had trouble coming to terms with the distributed model of manufacturing that Asos was suggesting – with production spread out around the country – and would rather have had manufacturing concentrated in just a few places.
But the most compelling factor was that while the talks were dragging on – with no sign that the government officials were close to a decision – many of the more than 200 individual health trusts around the UK opted not to wait for the outcome. Many decided to go “off piste”, as one participant in the talks put it, and place their own orders to top up supplies.
MIP – a big Canadian company which makes its gowns mostly in Asia – said it had committed to supply of 2m reusable gowns to UK health trusts in the first six months of 2020.
Alexandra, a UK based supplier of uniforms and other items of “workwear”, said that that at the peak of the Covid crisis it was selling as many as 2m gowns a month to trusts, split between reusable and single-use garments. In June it was selling around 500,000 a month in the UK, nearly all of which were made overseas.
.jpg) Sewing for Britain: the Northumbria Manufacturing and Distribution Hub has been among the most prominent groups to start making protective equipment for health workers
Sewing for Britain: the Northumbria Manufacturing and Distribution Hub has been among the most prominent groups to start making protective equipment for health workers
Several other schemes to source gowns involving individual health trusts and local manufacturers also started up.
Among the most prominent has been a scheme organised by the Northumbria Healthcare NHS Foundation Trust which led to the establishment of the Northumbria Manufacturing and Distribution Hub, led by Sarah Rose, a textiles executive. The hub, based in Cramlington, has made more than 650,000 disposable gowns for health trusts in north-east England using a network of factories.
.jpg) The failure of the mooted government initiative on reusable protective garments has been lambasted as “disappointing and frustrating"
The failure of the mooted government initiative on reusable protective garments has been lambasted as “disappointing and frustrating"
Due to the large numbers of gowns already bolstering local stockpiles, the cabinet office decided that a centralised scheme to make any sort of gown – either reusable or disposable – would lead to overstocking.
From now on, individual trusts will be left to procure gowns themselves, with some guidance from central government on specifications, along with encouragement to work with local industry partners where possible. It will be up to each trust to decide on the mix between throw-away and multi-use gowns.
The fall-out from the project’s messy end has been bruised feelings in industry. While Asos has not wanted to comment, its sourcing director Simon Platts is said by someone who knows him “not to be best pleased”.
Japanese textile maker Toray – which would have made most of the material for the project in a plant in Mansfield – said the cabinet office had been “slow and indecisive”. Had the government committed to the project Toray said it would have been ready to increase investment in its UK plant.
 Heathcoat Fabrics - with a big factory in Devon - was poised for a supporting role in the UK plan
Heathcoat Fabrics - with a big factory in Devon - was poised for a supporting role in the UK plan
Supporting roles could have been played by other UK-based makers of the specialised fabrics required for reusable gowns, such as Heathcoat Fabrics, which has a factory in Devon employing more than 400 people.
Heathcoat said the failure of the talks was “a huge opportunity missed to not only eliminate any future supply issues but to also help the domestic textile industry at a time when jobs and unemployment are going to be a key issue”.
 The reusables programme could have mobilised a large part of the UK textiles sector including this plant run by Heathcoat
The reusables programme could have mobilised a large part of the UK textiles sector including this plant run by Heathcoat
Life-saving clothing delivers a mountain of waste
Gowns used by medical staff to protect themselves from coronavirus are among the most vital elements of protective equipment and were used in vast numbers during the worst of the pandemic. They also generate huge amounts of waste.
Prior to the pandemic such gowns were required in the UK in only small quantities.
At the current rate of use – and on the assumption that gowns are predominantly disposable – medical gowns would generate more than 400 tonnes of waste a week, the equivalent of about 35 double-decker buses.
This is because under official guidelines protective gowns must be changed every few hours. Due to the scale of the pandemic, this meant individual hospitals required gowns in quantities barely imaginable to health planners before the crisis. Many health managers fear something similar could occur again in any new outbreak.
According to Cabinet Office estimates, at the peak of the pandemic, 460,000 gowns a day were being used in hospitals.
In recent years, most gowns and other items of personal protective equipment used in Britain have been single-use, mainly because extremely cheap disposable gowns have been available from low-cost countries.
Until prices rose sharply early this year, disposable gowns could be imported from China for about £1.50 each. Today the market price for single-use gowns sold in the UK (whether made locally or overseas) is £6-£10 compared to £8-£15 for reusable gowns.
Environmental advocates have however argued that basing policies solely on unit prices fail to consider other factors related to sustainability.
Christopher Nieper, managing director of the David Nieper clothes manufacturer, was among those who told Paul Deighton – head of government procurement efforts on PPE – that he should make a big effort to steer the UK away from disposable protective items in general and gowns in particular.
 The David Nieper clothes maker - a champion of “green manufacturing” in textiles - started its own project on reusable gowns
The David Nieper clothes maker - a champion of “green manufacturing” in textiles - started its own project on reusable gowns
“As well as being much better for the environment, reusable gowns are less expensive than disposables in the long run due to the number of times they can be returned for another wearing,” said Nieper. Early in the pandemic, his company switched much of its capacity to produce thousands of reusable gowns for sale to about 20 hospitals.
Nieper says his company’s gowns can be used 100 times between high-temperature washes. However, others say the number of uses per garment is on average much lower and could be just 25, depending on the quality of manufacturing and how the products are treated both during use and when washed.
On the basis that Britain needs to prepare for a long-term virus threat, the number of likely “gown uses” a year comes out at about 100m, according to the estimates likely to have been used by the Cabinet Office.
This number covers all possible uses, not just in hospitals but in other care and health settings including dentists and care homes. In a scenario where gowns are a mix of reusable and single-use garments, the 100m gown-uses can be met using a stock of gowns that becomes smaller as the amount of reusability in the mix increases.
For example, a nationwide stock of 10m washable gowns, each of them used an average of 40 times, would over their lifetimes provide 400m gown uses. Allowing for a generous buffer stock to provide time for cleaning and transportation, such a stock could be expected to account for a large proportion of the 100m annual number, requiring far fewer disposables.
by Peter Marsh
A sager stance on health hardware
The demise of an imaginative proposal to reset the UK’s approach to procuring personal protective equipment for health and care workers – based on reusability and domestic production – is extremely regrettable. It is tempting to regard this as simply another example of the government’s flawed decision-making during the pandemic. But the impulse simply to attack ministers and officials should be resisted. The project’s termination is a sorry episode. Yet it highlights key issues about the UK’s approach to public procurement, especially of health equipment. Understanding what went wrong could help Britain in the future, especially in an era where the threat of dangerous viral diseases is much greater.
It is impossible to overlook the government’s ham-fisted handling of the discussions. Having assembled an impressive range of people from textiles manufacturing and associated fields, officials were given a range of ideas on how a “reusable gowns project” might have worked. After lengthy conversations plus much work by textiles companies in testing fabric and producing samples, officials closed the discussions on the basis that the garments were no longer needed.
Despite this, these discussions have brought into sharper focus several key issues about the UK’s approach public procurement. Lessons can and should be learned.
Britain has placed too much reliance both on overseas producers, and on buying PPE such as gowns and masks on a “just in time” basis and holding minimum stocks. Particularly in the early days of the crisis, these factors left Britain woefully short of vital equipment. As a result, Britain was left in a weak position during the scramble to secure supplies from abroad. There are suspicions that suppliers and distributors – in the UK and overseas – capitalised on its weakness, forcing the UK authorities to overpay for essential supplies. The £15bn allocated by the Treasury for PPE during the pandemic suggests as much.
Britain’s focus on single-use PPE also looks increasingly out of step with 21st-century thinking on sustainability. In the past decade, the National Health Service has moved firmly away from reusable health equipment and towards items such as disposable gowns. Key factors have been the availability of such products at low prices from manufacturers in China, plus financial pressures placed on the UK health system by government austerity. The true costs of such hardware – especially considering the hidden impact of environmental degradation – have rarely been considered. It seems obvious that it is worth paying more for an item that can be used dozens of times than for one discarded after seeing service just once. Yet this is a rubric that the Department of Health and Social Care and the Treasury – responsible for NHS funding – seem not to prioritise. It is time they did.
All this said, the industry/government conversation about gowns shows how a dialogue between different groups can lead – potentially at least – to a viable project. The involvement of commercial laundry companies was especially important. Their message was that – contrary to what many believed – Britain has plenty of capacity and the expertise to build an effective 21st-century system based on reusable hospital clothing. Instead of regarding the attempt to do so by the Cabinet Office and business as a historical footnote, the government should use it as the basis for a renewed drive to put Britain’s system of PPE procurement on a secure and sensible footing.
